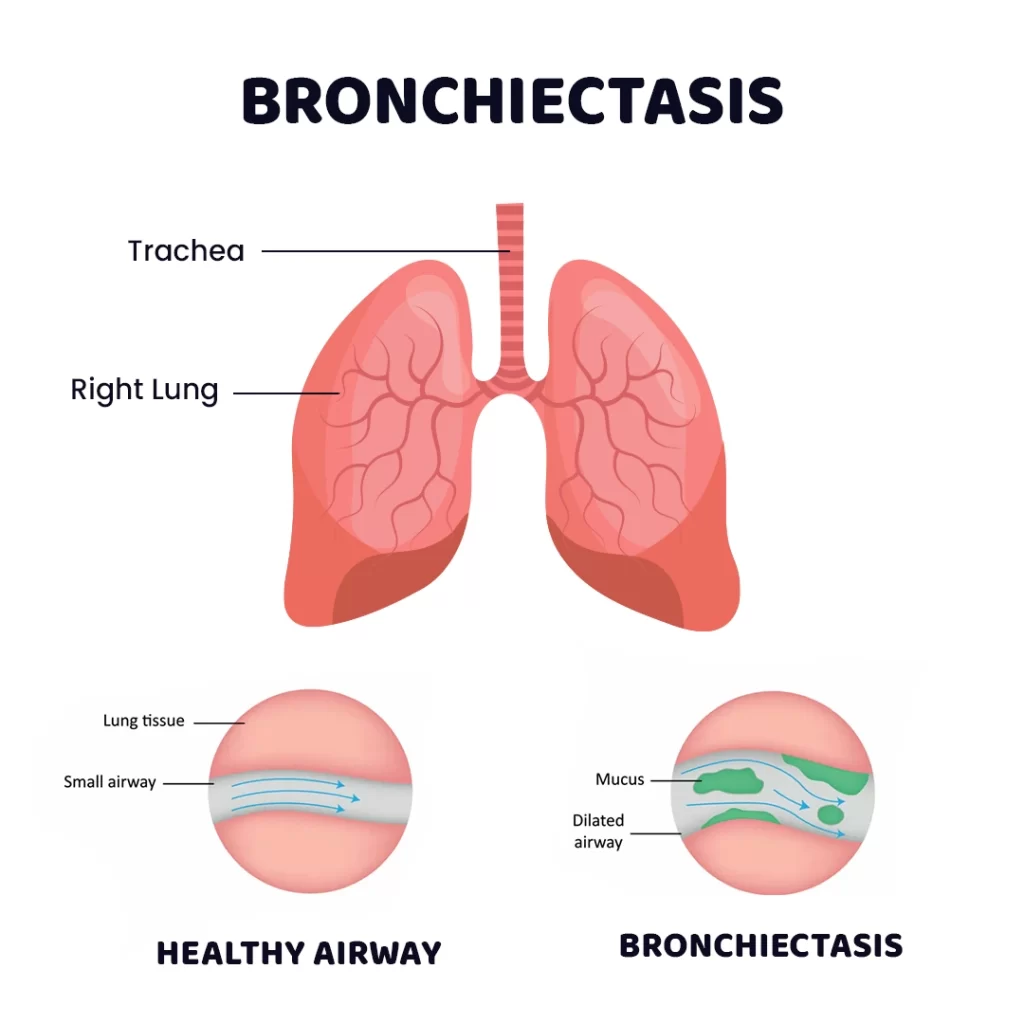
What is Bronchiectasis?
Bronchiectasis, also known as suppurative lung disease, is a condition where the airways inside the lungs become dilated, and the inner lining becomes swollen and diseased. This results in mucus buildup in the dilated airways, which leads to frequent lung infections. Repeated infections can further damage the airways, creating a cycle of progressive airway damage.
How is Bronchiectasis Different from Asthma?
While both bronchiectasis and asthma can cause cough and wheezing, they differ in underlying mechanisms:
- In asthma, the airways are inflamed and produce excess mucus, while the muscles around the airways tighten (bronchospasm). However, the airways are not dilated or permanently damaged.
- In bronchiectasis, the airways are dilated and damaged, and infection-related mucus build-up is the main issue. In some cases, a child may have both asthma and bronchiectasis.
What Causes Bronchiectasis in Children?
Common causes of childhood bronchiectasis include:
- Severe infections like pneumonia, tuberculosis (TB), whooping cough, or measles that damage the airways.
- Less common causes include cystic fibrosis, primary ciliary dyskinesia, immune deficiencies (e.g., common variable immunodeficiency, X-linked agammaglobulinemia), HIV, and allergic bronchopulmonary aspergillosis.
Signs and Symptoms of Bronchiectasis:
Children with bronchiectasis may show:
- A persistent, wet-sounding cough lasting for weeks or months due to mucus or phlegm buildup.
- Hemoptysis (coughing up blood) in some cases.
- Wheezing sounds similar to those in asthma.
- Poor weight gain and inadequate height.
- Exacerbations (flares) where symptoms worsen, including increased cough, yellow or green phlegm, fast breathing, and fever.
How is Bronchiectasis Diagnosed?
Diagnosing bronchiectasis usually involves:
- Chest X-ray (initial assessment, but may not confirm bronchiectasis).
- CT Scan of the chest (confirms bronchiectasis by showing airway dilation).
Additional tests may be needed to identify underlying causes:
- Immune deficiency tests
- HIV testing
- TB screening
- Allergic bronchopulmonary aspergillosis tests
- Sweat chloride test for cystic fibrosis
- Further investigations may include flexible bronchoscopy, sputum cultures, and pulmonary function tests.
Treatment for Bronchiectasis:
The primary treatments include:
- Chest physiotherapy to help clear mucus from the airways.
- Antibiotics for managing lung infections.
- Treating the underlying cause (e.g., addressing immune deficiencies, cystic fibrosis) is crucial to halt disease progression.
